Period Pain
Period pain can vary from very mild to pretty severe. While some people breeze through their monthly cycle, others have to curl up in bed with a hot water bottle and painkillers and wait until the cramps fade away. Generally, the pain is most intense during the first few days of your period. Cramps are felt in the lower abdomen, back and thighs and can seem worse at night. Heat compresses, gentle stretching and relaxation can help to ease period pain, as can non-prescription painkillers like paracetamol and ibuprofen. We understand the challenges of managing period pain. Let us support you with effective treatments to help you feel more comfortable during your menstrual cycle.
Period Pain Treatments
- Out Of Stock
 Feminax Express
Feminax Express - Out Of Stock
Mefenamic Acid 500mg Tablets
Mefenamic Acid 500mg Tablets - Out Of Stock

Panadol Period Pain Tablets (14)
Panadol Period Pain Tablets (14) - Out Of Stock
Evana Heavy Period Relief 500mg tablets
Evana Heavy Period Relief 500mg tablets - Out Of Stock
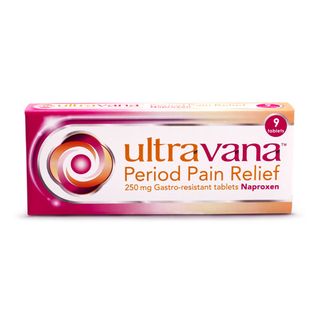
Ultravana Period Pain Relief 250mg Tablets
Ultravana Period Pain Relief 250mg Tablets
View recommended products for Period Pain
Don't wait to get the medical help you need.
View our recommended treatments and select your preferred treatment and quantity from a list of options for you.
- Selected by our UK-based medical team
- Quick and easy checkout
- Treatments dispatched same day (before 3pm)
Ordering as easy as 1, 2, 3
1. Find the ideal treatment
2. Get a free consultation
3. Enjoy speedy delivery
Advice for Period Pain
What is period pain?
Period pain – also called primary dysmenorrhoea – affects most women at some point during their lives.
As the name suggests, period pain is a pain suffered by women during their monthly periods. It usually presents as a discomforting cramping sensation in the lower muscles of the stomach, which can sometimes spread to the lower back and thighs.
The sensation of period pain can vary. For some women, the pain will come in intense spasms, whilst others experience a dull aching sensation instead. Period pain usually occurs at the same time as menstruation, and will normally last between 48-72 hours.
What causes period pain?
Period pain is caused by muscular contractions of the womb’s wall. During menstruation, these contractions become more intense, in order to encourage the wall to shed its lining.
These stronger contractions cause the wall of the womb to press against the surrounding blood vessels, briefly cutting off the womb’s blood supply. Without blood, the womb becomes temporarily deprived of oxygen, which causes the affected tissues to release a pain-triggering chemical. This, in turn, causes the body to produce another chemical called prostaglandins. Prostaglandins will cause the muscles in the womb to contract further, which will increase the intensity of the period pain even more.
In rare instances, period pain can be caused by an underlying medical condition. This kind of period pain is called secondary dysmenorrhoea. Some of the conditions that can cause secondary dysmenorrhoea include:
- Endometriosis: Where the cells that line the womb begin to develop elsewhere in the body, usually the ovaries and fallopian tubes. As these cells start to shed, they can cause intense pain.
- Pelvic inflammatory disease: A bacterial infection that affects the womb, causing it to become inflamed and irritated.
- Intrauterine devices: Also known as IUDs, these contraceptive devices are made from plastic and copper. Fitting inside the womb, they can sometimes cause period pain.
- Fibroids: is a condition caused by non-cancerous growths inside the womb. These benign tumours can make periods heavier and more painful.
Some women experience more period pain than others. The reason for this is still not entirely clear. However, it is suspected to be due to a build-up of prostaglandins, where some women appear to suffer a larger build-up than others. The higher the concentration of prostaglandins, the stronger the pain-inducing contractions will be.
What are the symptoms of period pain?
Period pain is a very common infliction. It is thought to affect up to 90% of menstruating women. The majority of cases will present as:
- Painful muscle cramps in the lower stomach
- Painful muscle cramps in the lower back and thighs
Period pain can be experienced as intense spasms, whilst for others, the pain will be more constant and dull. Other associated symptoms of period pain can include:
- Feeling nauseous
- Vomiting
- Backache
- Bloating
- Diarrhoea
- Headache or migraine
- Emotional symptoms, such as mood swings
If you are suffering from secondary dysmenorrhoea, you may also experience the following symptoms:
- Irregular periods
- Thick and unpleasant smelling vaginal discharge
- Bleeding in between periods
- Pain during sexual intercourse
Secondary dysmenorrhoea is more likely to develop as you get older. The majority of women affected are aged between 30-45 years old.
How is period pain diagnosed?
If your period patterns change significantly, it is advised to discuss your symptoms with your doctor.
To make an informed diagnosis, your doctor will ask about your symptoms and review your medical history. They will likely inquire as to how period pain is affecting your daily life. The next step is usually an examination of the abdomen. If unsatisfied, your doctor may arrange for a vaginal exam, where lubricated, gloved fingers are inserted into the vagina to check for abnormalities.
In some cases, a vaginal swab may be taken to rule out any sexually transmitted infections (STIs). If your doctor is still unable to make a diagnosis then further testing may be required. This could involve a pelvic ultrasound exam (using sound waves to produce an image of the inside of the abdomen), or a referral to a gynaecologist. If during any of the physical examination processes you experience any pain, it is important to relay this to your examiner.
How is period pain treated?
If suffering from secondary dysmenorrhoea, it will be important to identify the condition causing your symptoms before a suitable line of treatment can be discussed. However, if you suffer from primary dysmenorrhoea, there are several over-the-counter and prescription painkillers available to you.
For the majority of sufferers, period pain can be successfully treated at home using Non-Steroidal Anti-Inflammatory Drugs (NSAIDs):
Feminax Ultra 250mg: 9 tablets
- Provides period pain relief for up to 8 hours
- Suitable for women aged 15-50
- No prescription required
Feminax Express 342mg: 16 tablets
- Provides period pain relief after just 30 minutes
- Suitable for women and children aged 12+
- No prescription required
Mefenamic Acid 500mg: 9 tablets
- Fast-acting relief from period pain
- Suitable for women and children aged 14+
- Prescription is required
Warnings when taking period pain tablets
Taking tablets for period pain can help ease the discomfort caused by the muscular wall of your womb contracting. There are some things you need to keep in mind when taking this medication, though:
- Prolonged use of period pain tablets can lead to kidney and liver damage
- You shouldn’t take this medication if you have (or have had) a stomach ulcer
- Period pain tablets shouldn’t be taken while pregnant
- You should only take tablets at the recommended levels
If your period pain persists after taking painkillers for three months, speak to your doctor. They may refer you to a specialist for further tests to establish if you have an underlying medical condition. Along with a blood or urine test, these checks can include:
- A pelvic ultrasound: this checks for abnormalities in your reproductive organs.
- A laparoscopy: this checks your internal organs and takes tissue samples.
- A hysteroscopy: this uses a fiber-optic telescope to look for abnormalities.
Alternative treatments you can take for menstrual cramps
In addition to period pain tablets, other Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), such as ibuprofen, naproxen or cuprofen have proven effective at relieving period pain.
NSAIDs inhibit the production of prostaglandins, which is a chemical that causes the muscles in the womb to contract more severely during bouts of period pain. If NSAIDs are unsuitable, your doctor may recommend paracetamol instead.
A non-medicinal option for relieving period pain is transcutaneous electrical nerve stimulation (TENS). A TENS machine uses electrodes, which are placed on the skin at the site of pain. Electrical impulses are delivered through the electrodes, which is believed to interrupt the pain signals being sent to the brain.
Using heat patches and hot water bottles are effective ways of relieving period pain for many people. These are usually applied to the abdomen or the lower back. It is important not to apply heat directly to the skin, as it may damage it. Hot water bottles should only be used through clothes, and heat patches should only be applied as instructed by the manufacturer.
How do I prevent period pain?
Period pain isn’t always possible to prevent. However, there are some self-help techniques and lifestyle changes that can help reduce the symptoms from developing. These include:
- Exercise: aim to achieve 150 minutes + of moderate-intensity exercise each week. Any type of aerobic exercise will cause the body to pump more blood; which will result in the release of endorphins to counteract the prostaglandins. This will help ease the painful cramps.
- Stop smoking
- Reduce alcohol consumption: current guidelines recommend not exceeding 2-3 units of alcohol per day, with at least two alcohol-free days per week.
- Improve your sleep and relax more often
If these preventative measures don’t work, you can use medicinal treatments (such as period pain relief tablets) or natural remedies (like taking a warm bath) to ease the symptoms of your menstrual cramps.
FAQs for Period Pain
How long does period pain last?
Period pain normally begins at the onset of menstruation and generally doesn’t last for more than 2-3 days. The pain is usually at its worst when your bleeding is heaviest.What medicines can I use to treat period pain?
For the majority of sufferers, period pain can be successfully treated at home using over-the-counter painkillers, such as Ibuprofen and Aspirin. However, Ibuprofen and Aspirin should be avoided if you suffer from stomach or kidney problems, or if you have asthma. In these circumstances, Paracetamol would be the suitable alternative. If over-the-counter pain-relief is proving ineffective, your GP can prescribe you a stronger painkiller, such as Naproxen.Your doctor may suggest using the combined oral contraceptive pill. These pills can relieve period pain because they reduce the thickness of the womb’s lining. A thinner lining means the womb’s muscles do not have to contract as much in order to shed away your monthly period. The combined contraceptive pill also has the added benefit of reducing the amount of prostaglandins released by the body. Prostaglandins are pain-triggering chemicals.If the combined contraceptive pill proves to be unsuitable, contraceptive implants or injections may be a good alternative.What non-medicinal alternatives can I try for period pain?
There are several self-help techniques that can help relieve the symptoms of period pain. These include:- Exercise: exercising during a painful period can help reduce the discomfort. Exercise causes the release of endorphins, which help counter the pain triggering effect of prostaglandins.
- Stop smoking: smoking is believed to increase the risk of suffering from period pain.
- Heat therapy: applying a heat pad or hot water bottle can help reduce period pain. Always ensure hot water bottles are wrapped in a protective layer.
- Massage: gentle massage of the lower abdomen can help ease period pain.
- Relaxation: partaking in relaxing activities can help soothe the discomfort of period pain.
- Transcutaneous Electrical Nerve Stimulation (TENS): a compact battery-powered device that delivers mild electrical currents to the abdomen, which can help relieve pain.
Can period pain be prevented?
Sadly, period pain can’t always be prevented. Adopting a healthy lifestyle and practising self-help relaxation techniques is the best method for reducing the occurrences and severity of period pain.Do I need to see my GP about my period pain?
Period pain is perfectly normal. In fact, most women suffer some level of discomfort or pain during menstruation. However, if the cramping becomes severe, or if it is associated with nausea, diarrhoea, or headaches, then it is recommended to see your GP or gynaecologist.It is also recommended to speak with your GP should the normal patterns of your periods change significantly. For example, if your periods start to become irregular or heavier than what you are used to. In these circumstances, your doctor will likely run a few tests to check for possible underlying conditions that may be causing the irregular, painful periods. Possible underlying conditions include:- Endometriosis
- Pelvic inflammatory disease
- Fibroids
- Adenomyosis
Can period pain affect my fertility?
Period pain that’s caused by your natural monthly menstruation won’t affect your fertility. However, if the pain is being caused by an underlying condition, such as endometriosis, then there is a chance fertility may be affected.My mother suffers from period pain; will I suffer the same fate?
A family history of dysmenorrhoea can increase your risk. However, it can’t always be generalised, meaning there is a chance you won’t suffer the same levels of discomfort. You can actively reduce your risk by following a healthy diet, regular exercise, and practising stress-relieving techniques.