
Genital Warts
A type of human papillomavirus (HPV), genital warts are one of the most common sexually transmitted infections around. Unfortunately, genital warts are very contagious and can be passed on through pretty much all types of sexual activity. If you catch them, you’ll notice small, flesh-coloured bumps appear across your genitals. These warts have a cauliflower-like appearance and can spread pretty quickly. Luckily, we’ve got a range of creams and solutions that will support your body in fighting the virus and help your skin to heal fast.
Genital Warts Treatments
 Warticon Cream & Solution£29.99
Warticon Cream & Solution£29.99- Out Of Stock
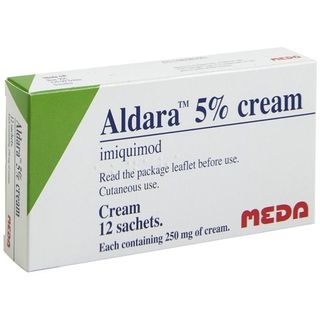
Aldara Cream
Aldara 5% Cream£74.99 - Out Of Stock

Catephen
Catephen 10% Ointment
Start your assessment for Genital Warts
Don't wait to get the medical help you need.
Once you complete a short online assessment about your condition, you will be able to select your preferred treatment and quantity from a list of appropriate options for you.
- Reviewed by our UK-based medical team
- Takes less than 3 minutes to complete
- Approved treatments dispatched same day (before 3pm)
Ordering as easy as 1, 2, 3
1. Find the ideal treatment
2. Get a free consultation
3. Enjoy speedy delivery
Advice for Genital Warts
Buy genital warts treatment from The Independent Pharmacy
If you’re wondering where to buy your genital wart treatments online, then you’ve come to the right place. It's easy, fill out an online form and our doctors will ensure it's the right genital warts treatment for you. The Independent Pharmacy provides all the medications, creams and advice you could need at the best price. We offer discreet UK delivery, straight to your door.
What are genital warts and what causes them?
In short, genital warts are caused by a type of human papillomavirus (HPV) and are among the most common types of sexually transmitted infections (STI).
Genital warts (condylomata acuminata) are the second most common sexually transmitted infection (STI) in England. They are caused by the human papilloma virus (HPV). They resemble small fleshy bumps on the skin and are found on and around the genital area. Genital warts usually don’t cause any pain or threat to health, however, they can look extremely unpleasant, which may cause emotional distress.
The papilloma virus that causes genital warts is passed from person to person through sexual contact. Both men and women can carry and pass on the virus. Unlike chlamydia, genital warts can be passed on through skin-to-skin contact, as well as penetrative sex. It is much more likely for the infection to spread if visible warts are already present. However, it is still possible to pass on a genital HPV infection even if warts have disappeared.
The virus is unable to pass through condoms, however, if the warts are on a part of the genitals not covered by the condom, then the infection can still be spread. They can spread to the anal area without necessarily engaging in anal sex. If partaking in oral sex, it is possible for the infection to develop in the mouth, although this is very rare. Papilloma virus symptoms cannot be spread from kissing, hugging or from sharing household objects, such as bath towels, toilet seats, plates and cutlery.
The papilloma virus that causes genital warts is passed from person to person through sexual contact. Both men and women can carry and pass on the virus.
Unlike Chlamydia, genital warts can be passed on through skin to skin contact as well as penetrative sex. It is much more likely for the infection to spread if visible warts are already present, though it is still possible to pass on the infection even if the warts have disappeared.
The virus is unable to pass through condoms, however, if the genital warts are on a part of the genitals not covered by the condom, then the infection can still be spread. Genital warts can spread to the anal area without necessarily engaging in anal sex. If partaking in oral sex, it is possible for the infection to develop in the mouth, although this is very rare. Genital warts cannot be spread from kissing, hugging or sharing household objects, such as bath towels, toilet seats, plates and cutlery.
The human papilloma virus belongs to a family of more than a hundred different viral strains. These different strains can affect different areas of the body. There are around thirty strains of HPV that can affect the genital skin. However, most of these strains rarely cause any visible symptoms. It is estimated that approximately ninety per cent of all genital wart cases are caused by just two strains of the HPV – type 6 and type 11.
What are the symptoms of Genital Warts?
The majority of people infected with HPV will not present with any visible warts or symptoms. The virus will usually go away on its own. If warts do develop it can take several weeks, months or even years, after initially coming into contact with the virus. When they do physically present they will typically appear as small fleshy bumps on the skin around the genital area.
They can appear singularly or in groups. When clustered together they can take on a ‘cauliflower’ type appearance. They also range in size, in many cases being so small that the sufferer won’t even notice them. The most common places to find genital warts differ between men and women.
For women, genital warts are usually found:
- Around the opening of the vagina (the vulva)
- In the neck of the womb (the cervix)
- Around and inside the anus
- On the upper thighs
In men, genital warts are usually found:
- On the penis
- On the scrotum
- Around and inside the anus
- On the upper thighs
- Inside the urethra
Genital warts are usually painless, in some cases, they can itch and become inflamed. Potentially, this can lead to bleeding from the anogenital area or urethra. If your flow of urine appears disrupted this may suggest the presence of genital warts in the urethra.
How are Genital Warts diagnosed?
It is recommended you pay a visit to your local sexual health clinic if you suspect you have genital warts for the first time. If a current or recent sexual partner develops the infection, you should also seek medical advice, even if you haven’t developed any warts yourself.
This venereal infection can be usually diagnosed through a simple visual examination. A doctor or nurse will examine the genital area to check for warts or changes to the skin around the genital area. As warts can be very small, the examiner may use a magnifying lens to help detect their presence.
If the warts are suspected in places not visually obvious, then a more detailed examination may be called for. This can include:
Vaginal examination
A vaginal examination is usually done using a vaginal speculum, which is a small plastic or metal tube. This device doesn’t cause any pain and will allow the doctor or nurse to see inside the vagina. A colposcopy will be performed if your pap smear results are unusual.
Anal examination:
An anal examination is usually performed with a device called a proctoscope. A proctoscope is a small plastic tube that will enable the doctor or nurse to examine the skin inside the anus. This examination is not usually painful.
Urethra Examination
If genital warts are suspected inside the urethra then it may be necessary to have a special examination of the urethra. This examination will need to be performed by a specialist.
After you have had your first outbreak of genital warts, you may never have another once they are successfully treated. If you do have another outbreak and the symptoms are the same, then it may be appropriate to self-diagnose and treat your warts. You should always see a healthcare professional if any of the following apply:
- The number of warts is significantly increased
- The size of the warts have increased
- The warts are a different colour or texture
- The warts appear in a different area
- You experience any new symptoms that were not present during your last diagnosis
How are Genital Warts treated?
The warts are usually treated with topical preparations such as Aldara Cream (imiquimod) and Warticon (Podophyllotoxin). You can buy both of these treatments from The Independent Pharmacy.
Treat genital warts with Aldara Cream
Aldara Cream contains the active ingredient Imiquimod. Aldara Cream is usually reserved to treat genital warts that are larger than normal.
It works by stimulating the immune system to attack the HPV infection. Aldara is applied directly onto the genital warts and left for six to ten hours before washing it off.
This process should be repeated three times a week. Aldara is suitable for treating warts around the genitals and anus.
Treat genital warts with Warticon 0.15% Cream
Warticon 0.15% Cream contains the active ingredient Podophyllotoxin. Podophyllotoxin is usually used when treating clusters of smaller warts.
Warticon works by poisoning the cells of the genital warts, killing them off. Warticon is used in cycles.
You start by applying the cream to the genital warts twice daily for three days. This is followed by a rest period of four days without treatment. Then the process is repeated again.
On average most sufferers using Podophyllotoxin (Warticon) will require four to five cycles to provide effective treatment. Warticon should only be used for external warts around the genitals.
Treat genital warts with Warticon 0.5% Solution
Warticon 0.5% Solution also contains podophyllotoxin. It can be used as an alternative to Warticon cream and is generally only used for males as the application of the solution can be harder to apply for females.
The treatment regime for Warticon solution is the same as the cream above, twice-daily applications for three days completed in weekly cycles. Warticon should only be used for external warts around the genitals.
There is also a range of less effective over-the-counter treatments available to treat your symptoms. However, we recommend that you seek medical advice and buy quality products from a reputable pharmacy like The Independent Pharmacy.
Physical treatments for genital warts
Should topical treatments prove ineffective then there are several physical techniques that can be considered by your GP. These include:
- Cryotherapy: Freezing warts using liquid nitrogen. Frozen warts should become inactive, and eventually fall off.
- Excision: This is where the warts are removed by cutting them away.
- Electrosurgery: using electric currents to burn away genital warts. Electrosurgery is a specialist treatment.
- Laser surgery: This is also a specialist treatment using a laser to burn away warts. This treatment is usually reserved for hard to reach genital warts, such as warts inside the anus and urethra.
Can I prevent Genital Warts?
By following the measure below you can significantly reduce your risk of developing genital warts and other sexually transmitted infections:
- Use condoms during vaginal and anal sex to prevent transmission. This will help protect against contagious conditions like genital warts and other sexually transmitted diseases. Using condoms will help prevent you from getting or passing on the HPV infection, especially if they are used while the warts are visibly present and for three months after they have disappeared. Without protection, you could easily give your infection to a partner.
- If engaging in oral sex, use a condom to cover the penis or a polyurethane square (dental dam) to cover the female genitals and anus.
- Avoid sharing sex toys where possible. Otherwise, ensure they are washed or covered with a fresh condom between users.
- If you’re a woman engaging in sex with another woman, use a soft polyurethane or latex square (dental dam) to cover your vulva when rubbing it against your partner’s vulva.
- The HPV vaccine( papilloma virus ) is now available and is given routinely to all girls in secondary school. Gardasil protects against most types of HPV including those that cause genital warts.
- Eat well, sleep well and exercise. HPV is a viral infection so it is important that your immune system is in good shape to fight off the infection.
FAQs for Genital Warts
What causes Genital Warts?
They are caused by the Human Papillomavirus (HPV). HPV is the name of a group of viruses that includes more than 150 different types that cause infection on the skin surface. Certain types of HPV cause warts on the hands or feet, while others can cause visible genital warts. Genital warts are specifically caused by HPV type 6 & 11.
What do Genital Warts look like?
The warts are small fleshy growths or bumps that can appear ‘cauliflower-shaped. For women, they can appear on the vulva, inside the vagina and on the cervix. For men, the warts can appear on the penis and scrotum. For both women and men, genital warts can affect the groin, thighs, and anus. They can range in colour from neutral skin-toned to brown or black.
Who gets Genital Warts?
If you are sexually active, evidence suggests that at some point during your life you will suffer with some form of HPV infection, though not necessarily genital warts. Most HPV infections will go unnoticed and will clear up spontaneously without the need for treatment.
How do you get HPV or Genital Warts?
Genital warts are usually spread by direct, skin-to-skin contact during vaginal or anal sex. It is also possible, but rare, to transmit them to the mouth by oral sex.
Warts on the hands and other areas of the body are caused by different strains of HPV, not the same ones responsible for genital warts. Contact with these warts on other areas of the body does not seem to cause genital warts.
I have some Genital Warts that have just appeared. Will my partner think I have cheated on them?
If you have unprotected sex with someone with genital warts, you are at risk of catching HPV and developing them yourself. You can still get genital warts even if you use a condom, depending on the area they affect in your sexual partner. Not everyone who is exposed to HPV 6 or 11 will go on to develop genital warts, however if you do they can take weeks or even months to develop. This can make it hard to know exactly when or from whom you got the virus.
How would I know if I had Genital Warts? Do they hurt?
External genital warts are normally noticed by either examining the area visually or by touch. In some cases in can be difficult to know, especially if the warts are flesh coloured. Sometimes people do not notice warts because they are inside the vagina, or on the cervix, or in the anus Only rarely do they cause symptoms such as itching, pain, or bleeding.
Sometimes genital warts will be found during an examination for a different condition. For women, an abnormal cervical smear may be the first warning sign that HPV is present, though a cervical smear is not a test for HPV.
Can I self-diagnose Genital Warts?
Genital warts can be normally be self-diagnosed after the first outbreak which should be reviewed by a healthcare professional. If you are in any doubt you should see your GP or local sexual health clinic for a formal diagnosis.
What should my partner do if I have Genital Warts or HPV?
Your partner should inspect themselves for signs of genital warts. If they have any visible external genital warts they should seek treatment. You should try to avoid sexual contact until both of your cases of genital warts have cleared up, however if this is not possible you should use a condom.
How are Genital Warts treated?
Genital warts don’t always require treatment; a lot of cases will slowly clear up on the own. However, due to the sensitive nature of the condition, which can often be unsightly and embarrassing, many people seek treatment to speed up the process. Treatment should aim to remove all the externally visible warts and hence also relieve any uncomfortable symptoms.
The available treatments for genital warts from The Independent Pharmacy are:
Podophyllotoxin (Warticon) - available as a solution and a cream. Warticon is applied twice daily for three days followed by a four day break, and continued for around four of these weekly cycles, though more may be necessary. Warticon burns away the wart tissue and removes each wart individually - it does not fight the HPV infection or reduce the chance of recurrence. The solution is normally recommended for men only as it is can be difficult for women to self-apply. Warticon cream may be more appropriate for women suffering with external genital warts.
Imiquimod (Aldara) cream can be used to treat external genital and perianal (around the groin and anus) warts. It is easy and safe to use for both males and females. Aldara is applied three times weekly for up to 16 weeks. Aldara stimulates the immune system to fight the HPV infection present in the skin. It can take longer to treat an outbreak of warts than Warticon, however treatment with Aldara cream has been shown to reduce the chances of a recurrent outbreak.
Treatment with Warticon or Aldara can take a number of weekly cycles so you must be patient during treatment.
If you are pregnant or think you might be, you should see your own GP for extra checks.
You should not use over-the-counter wart treatments that are not specifically for genital warts. These are not meant for sensitive genital skin.
It is recommended to avoid sexual contact with the infected area during treatment, to protect the treated area of skin from friction and help it heal.
Can HPV and Genital Warts be cured? Will I have them forever?
Genital wart treatment aims to remove the external warts but it does not kill the HPV virus. This means that in some cases the virus can lie dormant and recur at a later date, although this is not always the case. It can take several treatment cycles to completely get rid of genital warts. Unfortunately there is no cure for HPV itself.
What about HPV, cancer and Genital Warts?
The strains of HPV linked to cervical cancer are not usually the types linked with genital warts (HPV 6 & 11). However, a woman with genital warts, like any other sexually active woman, should have regular smears to check their cervix.
HPV immunisation and regular cervical smears are the best safeguard against cervical cancer. Cervical smears detect abnormal cells present on the surface of the cervix. Cancer almost always can be prevented through the early detection and treatment of abnormal cervical tissue.
What about HPV, Genital Warts and pregnancy? Is getting pregnant dangerous?
Genital warts very rarely cause problems during pregnancy and delivery. However due to changes in the body during pregnancy, warts can grow in size and number. If you have genital warts or think you may have been exposed to genital warts and you are or may be pregnant, you should see your GP for further advice and treatment. In very rare cases, it is advisable for pregnant women to have a C-section over a natural birth for the wellbeing of mother and baby.
What are filiform warts and why are they formed?
Filiform growths are long, thin and flesh-coloured warts that can be found on the face, eyelids, neck or lips. These warts can form then a strain of HPV makes the top layer of your skin grow too rapidly.
Can you catch these warts from a toilet seat?
It is important to be aware of how the HPV virus can be contracted. However, you cannot get genital warts from any of the following:
- Close physical contact when clothed, such as hugging or sharing baths or towels
- Kissing
- Using swimming pools
- Sharing cups, plates or cutlery
Do Genital Warts smell?
Genital warts are generally odourless. However, ulcerated warts or infected areas of skin may produce a discharge with an unpleasant odour if not treated urgently.
How long does it take for the warts to go?
Treatment can generally clear warts within 3 months, however, it is a topic of debate whether this clearance means that there is still a residual inactive virus or that all the virus has been completely eradicated. Methods such as diathermy, laser ablation and excision will have an immediate effect, as any of these approaches can remove genital warts and lesions in just one treatment. Patients with 1-3 warts generally require fewer treatments and less treatment time than those with more lesions.
You may require more than one course of treatment. If your symptoms persist, contact a healthcare professional for advice.
Why do people who do not have anal sex sometimes get anal warts?
Anal warts can commonly occur in the absence of anal intercourse. This is because HPV is typically multi-centric and is not limited to the original site of infection. HPV can be transferred in a number of ways, for example by fingers from the genital to anal epithelium during foreplay.
Can Genital Warts lead to infertility?
The warts themselves should not affect your chances of getting pregnant. However, the HPV virus can increase your risk of developing precancerous or cancerous cells in your cervix. This could affect your fertility and ability to carry a child to term.
Is any gender more likely to get Genital Warts?
You are equally likely to contract HPV and suffer from genital warts regardless of whether you are a man, woman or of any other gender identity.